- What do I need treatment for?
- Before the treatment
- Coming into hospital
- The anaesthetic
- The operation
- Recovery and aftercare
- Going home
- Are there any complications?
- What can I do to help myself?
What do I need treatment for?
As your vascular surgeon has explained to you, the main artery in your abdomen, the abdominal aorta, has a weak and swollen area (abdominal aortic aneurysm). In order to prevent bursting (rupture) of the aneurysm, you need to have an operation for replacement of this part of the aorta with a graft.
This method was selected in your case as a better option over endovascular repair either because the anatomical features (shape, extent, relation to the renal arteries etc) of your aneurysm are not favourable for repair with a stented graft (EVAR) or on grounds of your age and medical history.
Before the treatment
Before the operation is performed, certain investigations and tests need to be done. These are of two kinds:
(i) The ones used for assessment of your general health state and your suitability for the operation. These are normally done before a final decision is made regarding the type of procedure you will have, and include blood tests, electrocardiography, echocardiography, chest x-ray, lung spirometry (measurement of lung function reserve) etc. Evidently, CT angiography of the aorta and the iliac arteries will have already been performed.
(ii) The ones done on admission usually the day before the operation, including bood tests and a new electrocardiogram
Your physician will generally request that 2-4 units of blood be available for you. In Greece, you need to personally liaise with the Blood Bank of your hospital in order that blood is secured for you.
The physician will have probably asked you to discontinue for a few days (if you take) any anticoagulant, like Warfarin or Sintrom, or antiplatelet drugs like Clopidogrel (Iscover, Plavix) or Aspirin, in order to reduce the risk for bleeding.
Coming into hospital
When you are admitted, it will be quite useful to bring with you all medications you are on. Your medical history will be recorded. Later, your vascular surgeon and the anaesthetist who will put you to sleep will visit. They will explain certain aspects of the procedure and of the immediate postoperative care you will receive at the Intensive Care Unit. You will be asked to sign a form confirming that you understand why the procedure needs to be performed, the risks of the procedure and that you agree to the surgery.
The anaesthetic
The first part of any operation is the administration of anaesthesia. Initially, your anaesthetist will probably insert an epidural catheter in your back to provide pain relief during and after the operation. Through an IV in your arm, used to provide you with fluids and medications, you will receive the anaesthetic which will put you to sleep within a few seconds. Then, a “central” venous catherer will probably be inserted in a large vein in your neck to give you the fluids required during and after the operation, and an “arterial line” will be used for continuous monitoring of your blood pressure. A urinary catheter will be placed in your bladder to monitor your urine output. Sometimes, a nasogastric tube (passed through a nostril into your stomach) is placed to prevent nausea and vomiting after the operation.
The operation
A large incision will be done in your abdomen and – if necessary – two smaller ones in your groin areas. After control of blood flow in the aorta has been achieved, the weakened part of your aorta with the aneurysm is incised and opened. It will be replaced with a graft, or a plastic tube, which allows your blood to flow through it.
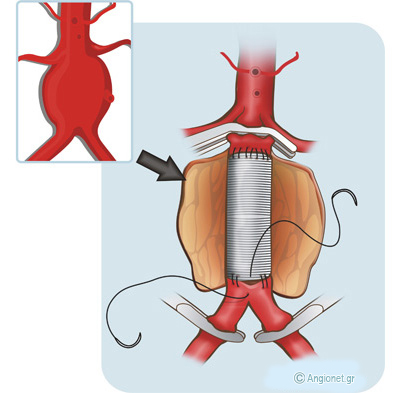
The graft (white colour) replaces the aneurysmal part of the aorta. The way of sewing the graft to the normal (non-aneurysmal) wall is shown
The graft is made of very strong durable plastic material, either Dacron (polyester) or PTFE (polytetrafluorethylene) in the size of normal aorta, and is either straight or bifurcated. Then, the redundant sac of the aneurysm will be sewn to cover the graft. The wounds will be closed either with nylon stitches or metal clips, which will be removed in 10-12 days, or with absorbable sutures.
The graft lasts for a lifetime and is very unlikely to require replacement. The operation is successful in 95-98% of cases.
Recovery and aftercare
Following the operation you will be transferred to the Intensive Care Unit (or High Dependency Unit) for closer observation, where you wil stay for 24-48 hours. Occasionally, you need to remain intubated for a while, but efforts will be made to reduce this period to the minimum. There, you may also start chest physiotherapy.
After this operation, it is common for the bowels to stop working for a few days and during this period you will be given all your fluids with a drip. It may be necessary for you to have a blood transfusion. The nursing and medical staff will try to keep you free of pain and will explain you how.
Over the next few days as you start to recover, the various tubes will be removed and you will return to the normal ward until you are fit enough to go home (usually 5-8 days after the operation).
You will be given a small injection every day to lower your chance of getting a deep vein thrombosis or pulmonary embolus after the operation. These will continue until you are fully mobile and discharged from hospital.
Going home
You will often feel tired but this will improve as time goes by. It will take you 2-3 months to fully recover but this period depends upon your age.
- Your physician will advise you to regularly go for short walks and then rest for gradual return to normal activities
- You can have a bath and wet the wound(s) a few days after the operation
- You will be able to drive when you can perform an emergency stop safely. This will be 3-4 weeks after the operation
- You should avoid lifting weights for 6 weeks
- If you work, you should be able to return to work in 6-12 weeks
- You will usually be recommended to take Aspirin or Clopidogrel (Iscover, Plavix) and a statin, as you probably did before the operation
Are there any complications?
– As with any major operation there is a small risk of you having a medical complication, such heart attack, stroke or chest problems
– After this particular operation, you may get kidney failure or loss of circulation in the legs or bowel
– Chest infection may happen especially in smokers, and chest physiotherapy and/or antibiotics may be required
– The surgical wounds may get infected and require antibiotics. Serious infections, however, are rare
– Infection in the artificial artery is very rare (1 in 500). This is a very serious complication requiring replacement of the graft
– Collection or leak of fluid (lymph) in the wound in the groin. It usually settles down by itself within weeks
– The bowels may stop working for a few days and during this period you will be given all your fluids via a vein drip
– Sexual incompetence (problem with erection or ejaculation) or retrograde ejaculation (the semen travels up into your bladder instead of coming out your penis, but it does come out later when you urinate). These may occur in men (about 10%), because occasionally it may be unavoidable during the operation to cut some small nerves running in front of the aneurusm
Each of these complications is rare, but overall it does mean that some patients may not survive their operation or the immediate post-operative period. For most patients this risk is up to 5% from an open aneurysm repair – in other words 95 in every 100 patients will make a full recovery from the operation. Your medical team will take all precautions to prevent any problem and try to correct it as early as possible.
If your risk of a major complication is higher than average, usually because you suffer from a serious medical problem, your vascular surgeon will discuss it with you. It is important to remember that your vascular surgeon will recommend the operation only if he/she believes that the risk of aneurysm ruprure is greater than the risk posed by the operation itself.
What can I do to help myself?
You should make changes in your lifestyle to help avert the chances to further damage your arteries. If you don’t, you are at increased risk for a heart attack, a stroke or problems with the circulation to your feet.
These changes include:
- Quitting smoking completely
- Exercising aerobically, such as brisk walking, for 25 to 30 minutes daily
- Maintaining your ideal body weight
- Eating foods low in animal fat, cholesterol, and calories
- Taking your medication to control blood pressure, blood cholesterol and diabetes
Last modified 09/09/2016