- What is a leg ulcer?
- What causes leg ulcers?
- What are the symptoms?
- How is the diagnosis of the cause of an ulcer made?
- How will I be treated?
- How long will it take the ulcer to heal?
- Is there any risk of losing my leg?
- What can I do to help myself?
- How can I prevent the ulcer coming back?
What is a leg ulcer?
An ulcer (or a sore) is simply a break in the skin. The immediate cause is usually a small injury on the calf or the foot that breaks the skin. If there is an underlying problem, the skin cannot heal normally (i.e. in less than 2 weeks), and the wound can increase in size. This is a chronic or nonhealing ulcer.
Leg ulcers are more common in women and in the elderly. They are responsible for physical disability and loss of many hours of work for many people. If left without treatment, they may end up in leg loss.
What causes leg ulcers?
Venous ulcers (caused by venous stasis) – These constitute over 70% of all leg ulcers. Every time you move your calf muscles, blood is pumped from the foot to the heart through your veins, which are tubes having one-way valves that make sure the blood goes up the leg and never back down. In some people, these valves are not very effective or can be damaged by thrombosis (clots) in the veins. Then, blood flows back down the leg and increases the pressure in the veins, which in turn will gradually stretch and leak fluid at the level of the capillaries. This abnormality causes swelling, damages the skin and leads to the ulcers (chronic venous insufficiency).
In this ulcer category, we can also classify the relatively rare ulcers caused by lymphoedema or by oedema in congestive heart failure, since their management is similar.
Arterial or Ischaemic ulcers (caused by poor circulation) – These constitute about 10-15% of all leg ulcers. The arteries of the legs bring oxygenated blood down to the foot. If the arteries get narrowed or blocked, usually in relation to atherosclerosis (peripheral occlusive arterial disease), caused by smoking, diabetes, high blood pressure or high cholesterol, the circulation to the leg may be significantly reduced. Hence, tissues are in lack of oxygen and nutrients, the skin is vulnerable to injuries and its healing potential reduced.
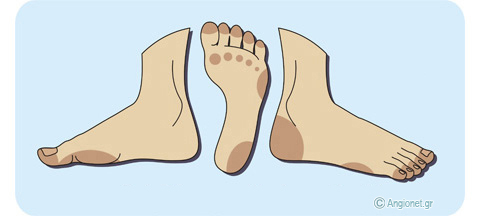
Neuropathic or Neurotrophic ulcers (common in diabetics) – It is estimated that 15% of all diabetics will develop a foot ulcer during their lifetime, usually on the sole of the foot or the toes. Diabetes mellitus is a risk factor for peripheral occlusive arterial disease. On the other hand, it may damage some nerves in the legs (diabetic neuropathy) causing loss of feeling in their lower part putting them at increased risk for ulcerations. According to the underlying cause, foot ulcers in diabetics may be purely neuropathic, neuro-ischaemic or purely ischaemic (arterial). Ulcers in diabetics may be aggravated by smoking, malnutrition, poor control of diabetes, poor foot care and unsuitable shoes.
A special category of ulcers are the pressure ulcers, caused by long-standing pressure on a certain area of the skin (e.g. heel, achilles tendon, coccyx) commonly in individuals which are bed-ridden or have significant mobility disabilities, without evidence of vascular disease or diabetic neuropathy.
Rare types of ulcers – About 5% of all leg ulcers have a rare cause. Such causes may be angiitis (e.g. in rheumatic diseases, such as scleroderma or lupus erythematosus), states with cryoglobulinaemia (in myelo-proliferative disorders, like polycythaemia rubra vera, or in certain chronic inflammatory conditions), certain congenital blood disorders, drug induced (e.g. hydroxyurea), gangrenous pyoderma (e.g. in ulcerative colitis), osteomyelitis, skin malignancy etc.
In some cases two or more conditions may be causing damage at the same time, and then we talk about mixed (or multifactorial) ulcers. For example, if there is poor arterial circulation in a leg with a venous ulcer, arterial surgery may be required first to improve the blood supply, thus offering the healing potential, before the ulcer starts to heal.
What are the symptoms?
Some leg ulcers produce fluids, especially if there is leg swelling. These fluids may be foul smelling. This wet environment favours the development of bacterial infections of the skin and subcutaneous fat, and antibiotic treatment may be necessary.
Venous ulcers – These lesions typically occur in the medial aspect of the leg around the ankle, where venous pressure is maximal and large perforating veins are present.
The leg may be swollen and tender to the touch. Lipodermatosclerosis, i.e. fibrosis of the skin and subcutaneous tissues, develops. The surrounding skin may have a reddish or brown-black discolouration and areas of white atrophy (or “atrophie blanche”) may be present. The skin is dry and itchy.
Some venous ulcers are painful, especially when they are infected.
Arterial ulcers – These tend to develop in the lower part of the leg and the foot. The foot is usually cold and, depending on the position it is examined (eleveted or dependent), it may have either a pale or a red-purple, shiny appearance.
Arterial ulcers are usually very painful, especially in bed at night. The pain is often ameliorated a little with leg dependency.
Diabetic neuropathy ulcers – These develop in the vulnerable areas of the leg and foot, and are usually painless. This is one of the features of the diabetic foot.
How is the diagnosis of the cause of an ulcer made?
Diagnosis of the type (cause) of a leg ulcer is based on the appearance and the location of the ulcer. However, additional information from the medical history and the physical examination may be required. To rule out poor circulation as a cause of the ulcer, it is common to compare the systolic blood pressure at ankle level to the systolic blood pressure of the arm, and find the ratio called ankle-brachial pressure index (ABPI). A hand-held Doppler and a manometer are required for these measurements to be done.
Patients with venous or arterial ulcers can further have duplex ultrasonography of their leg veins and arteries. In arterial ulcers, to study the leg arteries and plan operative treatment, a special x-ray of the arteries, such as CT angiography and digital subtractive angiography, is usually required.
How will I be treated?
Remember that a leg ulcer is like any other wound: it has to heal up within a week or two. If this does not happen in your case, see your doctor. The earlier you tackle the problem, the easier the ulcer will heal and with a better outcome. Never wait for a month or two until you consult a specialist! Otherwise, the treatment may be more complicated and the outcome less satisfactory. As specialists in treating leg ulcers caused by vascular disorders, we use various tecniques.
The mainstay of treatment of a venous ulcer is reduction of the high pressure in the veins of the leg and of the ulcer itself.
– Elevation of the leg. Put your legs up whenever you can. Elevate the lower end of your bed (about 15 cm) so that when in bed your feet are a little higher than your head.
– Compression bandaging or stockings. In order to keep the pressure in the leg veins at the ankle low when you are standing up, you will be treated with compression using several layers of bandages to get the necessary pressure to control the veins. Once the ulcer is healed, compression stockings are usually necessary to prevent the ulcer from returning.
– Wound dressings. Each time you have a wound change, suitable dressings will be applied. Their choice depends upon the phase of wound healing, therefore, dressings may differ from time to time.
– Surgery. In some cases a suitable operation may be the cure, as in ulcer related to superficial venous disease, when varicose vein surgery is required. Another possibility may be skin grafting on the ulcer.
In arterial ulcers, the aim is to increase blood flow to the foot. This may be achieved with arterial bypass surgery (placing a graft, i.e. a new artery) or balloon angioplasty (opening an artery by inflating a special balloon in it).
Occasionally, antibiotic therapy may be necessary to manage an ulcer, particularly if there are signs of infection in the surrounding skin and tissues.
The management of mixed ulcers may be more complicated.
How long will it take the ulcer to heal?
Since it has usually taken many years for the chronic venous insufficiency to cause the ulcer, it is not surprising that the ulcer may take a long time to heal. Although most venous ulcers will have healed within 3 months, in a small percentage it will take longer. Even in these resistant cases, treatment should eventually be successful.
Is there any risk of losing my leg?
It is extremely rare for a venous ulcer to lead to leg amputation since even large ulcers can be treated successfully.
An arterial ulcer will usually heal, if it is feasible to perform a procedure to increase blood flow to the foot. However, in case the vascular surgeon assures you that revascularization, or improvement of circulation, cannot be done, especially if there is severe pain, it may be better to decide to have an amputation.
The various ulcers (neuropathic, neuroischaemic and ischaemic) which diabetic people may develop in their legs, require immediate attention and care by a specialist because these may threaten the viability of the leg. It is estimated that 14-24% of diabetics with a foot ulcer will require an amputation.
What can I do to help myself?
- Quit smoking
- Have a healthy diet
- Exercise aerobically (e.g. brisk walk). Avoid sedentary life and prolonged standing
- Wear surgical stockings, if your physician has recommended so
- Avoid tight clothes and use comfortable shoes
- Protect the skin of your legs and check it carefully every day
How can I prevent the ulcer coming back?
It is true that ulcers tend to return, especially in the elderly.
In the cases when surgical correction of the underlying disorder is feasible, surgery commonly prevents ulcer recurrence.
If the underlying problem persists, you need to take certain measures so that the ulcer doesn’t come back. If you are advised to wear compression stockings, you need to wear them indefinetely and replace them every 3-4 months when they lose the degree of compression pressure that they are made to exert.
People with diabetes should carefully follow the instructions for diabetic foot care.
Last modified 03/03/2015