- What do I need treatment for?
- Before the treatment
- Coming into hospital
- The anaethetic
- The operation
- What can I expect after the operation?
- Going home and aftercare
- Are there any complications?
- What can I do to help myself?
What do I need treatment for?
As your vascular surgeon has explained to you, it was found that you have a medical problem related to a very narrow or blocked artery usually due to atherosclerosis (or hardening of the arteries), which affects the arteries of your leg(s), and is called peripheral occlusive arterial disease. This blockage reduces the blood flow to your limb to such a low level that its function is affected either causing you symptoms, such as disabling intermittent claudication, or putting the viability of your foot at risk, as in critical limb ischaemia.
Based on your medical history, physical examination and imaging investigations, it is very likely that the circulation to your leg will be improved with an operation bypassing the blockage with a graft, so that a new artery for blood flow to your leg is created.
Before the treatment
Before the operation is performed, certain investigations and tests need to be done. These are of two kinds:
(i) The ones used for assessment of your general health state and your suitability for the operation. These are normally done before a final decision is made regarding the type of procedure you will have, and may include blood tests, electrocardiography, echocardiography, chest x-ray, lung spirometry (measurement of lung function reserve). Evidently, tests to image your leg arteries, such as duplex ultrasonography, digital subtractive angiography and CT angiography will have already been performed
(ii) The ones done on admission usually the day before the operation, including bood tests and a new electrocardiogram
Your physician will generally request that 2-4 units of blood be available for you. In Greece, you need to personally liaise with the Blood Bank of your hospital in order that blood is secured for you.
The physician will have probably asked you to discontinue for a few days (if you take) any anticoagulant, like Warfarin or Sintrom, or antiplatelet drugs like Clopidogrel (Iscover, Plavix) or Aspirin, in order to reduce the risk for bleeding.
Coming into hospital
When you are admitted, it will be quite useful to bring with you all medications you are on. Your medical history will be recorded. Later, your vascular surgeon and the anaesthetist who will put you to sleep will visit. They will explain certain aspects of the procedure and of the immediate postoperative care. You will be asked to sign a form confirming that you understand why the procedure needs to be performed, the risks of the procedure and that you agree to the surgery.
The anaethetic
The first part of any operation is the administration of anaesthesia which may be regional, general or a combination of the two. Initially, your anaesthetist will probably insert an epidural catheter in your back to provide pain relief during and after the operation. Through an IV in your arm, used to provide you with fluids and medications, you may receive the anaesthetic which will put you to sleep within a few seconds. Then, a venous catherer will be inserted in a large vein to give you the fluids required during and after the operation, and an “arterial line” will be used for continuous monitoring of your blood pressure. A urinary catheter will be placed in your bladder to monitor your urine output.
The operation
The exact type of procedure depends upon your symptoms, your general state of health and the extend of the damage of your arteries. The bypass operation in named after the names of the arteries connected, e.g. aorto-femoral, axillo-femoral, femoro-popliteal, femoro-tibial.
In general, a skin incision is made at or above the level of the artery which has the blockage. After dissecting the artery, the vascular surgeon will assess the pulse of its healthy part. This way, it is essentially confirmed that the artery can be used to provide good blood suply to the bypass graft to be connected to it. The graft is selected accorging to the type and site of the procedure. It may be either natural (one of your veins) or artificial (synthetic).
The long saphenous vein, lying under the skin of each leg from the ankle to the groin, is the venous graft of choice. The synthetic grafts are made of very strong, durable plastic material, either Dacron (polyester) or PTFE (polytetrafluorethylene) in the size of normal arteries.
Then, the surgeon makes another skin incision, as required, opens the artery above and below the blockage, and implants the graft with a standard technique sewing it to both areas of the artery, above and below the blockage.
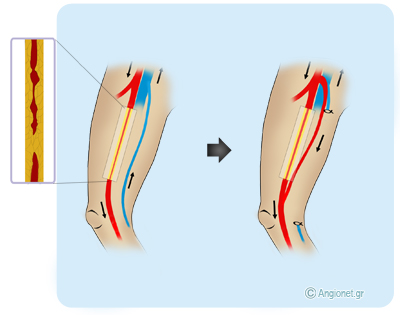
In the figure, the superficial femoral artery (red colour) is shown with a long occlusion. In order that a bypass of the blockage is performed, a segment of the long saphenous vein (blue colour), which lies beside the artery in a parallel course, is used. The arrows show the direction of blood flow.
The surgeon may assess the functional result of the procedure while still in the operating theatre with on-table angiography or Doppler ultrasound. Finally, the wounds will be closed either with nylon stitches or metal clips, which will be removed in 10-14 days, or with absorbable sutures.
What can I expect after the operation?
Following the operation you may be transferred to the High Dependency Unit for closer observation, where you will stay for 24 hours, and then you will return to your normal ward. Over the next few days as you start to recover, the various tubes will be removed and you should be fit enough to go home usually 3-8 days after the operation. Your vascular surgeon will be monitoring the result of the operation and ensure it’s working properly.
If an incision in your abdomen was done, it is common for the bowels to stop working for a few days and during this period you will be given all your fluids with a drip. It may be necessary for you to have a blood transfusion. The nursing and medical staff will try to keep you free of pain and will explain you how.
You will be given a small injection every day to lower your chance of getting a deep vein thrombosis or pulmonary embolus after the operation. These will continue until you are fully mobile and discharged from hospital.
Going home and aftercare
Initially, you may require physiotherapy or assistance by another person. Your physician will advise you to regularly go for short walks and then rest for gradual return to normal activities. You will usually be recommended to take Aspirin or Clopidogrel (Iscover, Plavix) and a statin, as you probably did before the operation.
If any incision gets red, swollen or is leaking, if you develop fever or if the foot of the side of the operation gets cold or numb, you should immediately contact your physician, because a complication may have occured.
Are there any complications?
Like in any major operation, there are risks related to the anaesthetic and to the operation itself.
– Swelling of the operated leg is almost unavoidable and isn’t necessarily a complication. A collection or leak of fluid (lymph) may occur in the wound in the groin. It usually settles down by itself within weeks. The wound(s) may occasionally get infected and require antibiotics.
– The graft can rarely get infected, bleed or get blocked. These are serious complications which may require prolonged antibiotics or further surgery and could eventually lead to loss of the leg.
– If you have had an aortic procedure, the bowels may stop working for a few days and during this period you will be given all your fluids via a vein drip. Also, younger men having this type of procedure should discuss with their vascular surgeon the possible impact of the operation on their sex life.
– Chest infection may happen especially in smokers, and chest physiotherapy and/or antibiotics may be required.
– There is potential risk for a serious complication, such as heart attack, stroke, kidney failure, chest problems or loss of circulation to the bowel (in case of an aortic procedure). All these complications are rare.
What can I do to help myself?
Your procedure does not stop plaque build up. If you have had an arterial bypass procedure, you should make changes in your lifestyle to preserve its success and help avert the chances to further damage your arteries. If you don’t, you are at increased risk for a heart attack, a stroke or further problems with the circulation to your feet.
These changes include:
- Quitting smoking completely
- Exercising aerobically, such as brisk walking, for 25 to 30 minutes daily
- Maintaining your ideal body weight
- Eating foods low in animal fat, cholesterol, and calories
- Taking your medication to control blood pressure, blood cholesterol and diabetes
Last modified 09/09/2016